Does scopolamine increase perioperative mortality?
Anticholinergic medications have long been part of the Beers Criteria, a list of medications to avoid or use with caution in older adults. The main concerns are an association between their use and an increased risk of dementia and, in the short term, delirium. While scopolamine is widely used to prevent postoperative nausea and vomiting (PONV), does it increase the risk of postoperative complications including mortality?
A 2024 paper looked at whether scopolamine use was associated with an increased risk of delirium and mortality, among other outcomes, within seven days postoperatively. Patients who underwent inpatient or outpatient surgery (urology, colorectal, orthopedics, neurosurgery, vascular, and thoracic) and received scopolamine within 24 hours of surgery were enrolled. Exclusion criteria included cardiac surgery, patients in the ICU, palliative care patients, and those who had received scopolamine or antipsychotics within the prior three months.
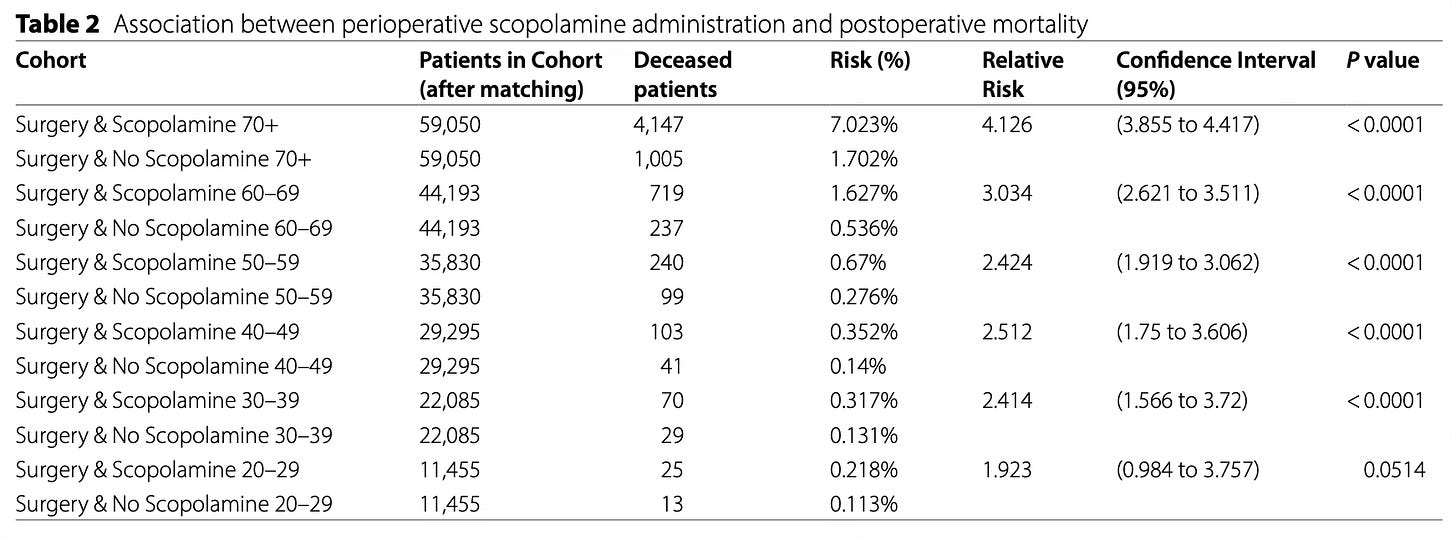
Individuals were grouped into cohorts by age (20-29 years, 30-39 years, … 70+ years) and propensity score matched to yield 201,908 pairs. Across all age cohorts scopolamine use was associated with increased postoperative mortality. The relative risk of mortality increased with increasing age cohort. Among those aged 30-39 years, the relative risk was 2.414 (p < 0.0001). Among the 70+ cohort, the relative risk of 7-day postoperative mortality was 4.126 (p < 0.0001). Only the 20-29 cohort was not statistically significant (RR 1.923, 95% CI 0.984-3.757, p = 0.0514); this cohort also had the least number of individuals and may have been underpowered to detect a difference.
The authors only found a statistically significant increased rate of delirium in those aged 60+ years. However, scopolamine use was associated with new antipsychotic use across every cohort which could suggest that delirium was more prevalent than was recorded in the database from which the data was gathered. When looking at other complications, the risk of readmission was higher in the scopolamine group across all cohorts except those aged 20-29 years, and the risk of urinary retention was increased across all cohorts.
Perhaps the biggest limitation with this paper is that scopolamine dose, route of administration, and duration of use were not evaluated. The inclusion criteria of scopolamine within 24 hours of surgery leads one to reasonably assume it was administered as a patch for prevention of PONV, yet the route and total dose remain a major limitation. In the absence of a randomized controlled trial which may never occur, this evidence was enough for me to stop using scopolamine.
Given these complications, and the many alternative drugs to prevent and treat PONV, the time has come to retire scopolamine in favor of safer antiemetics.